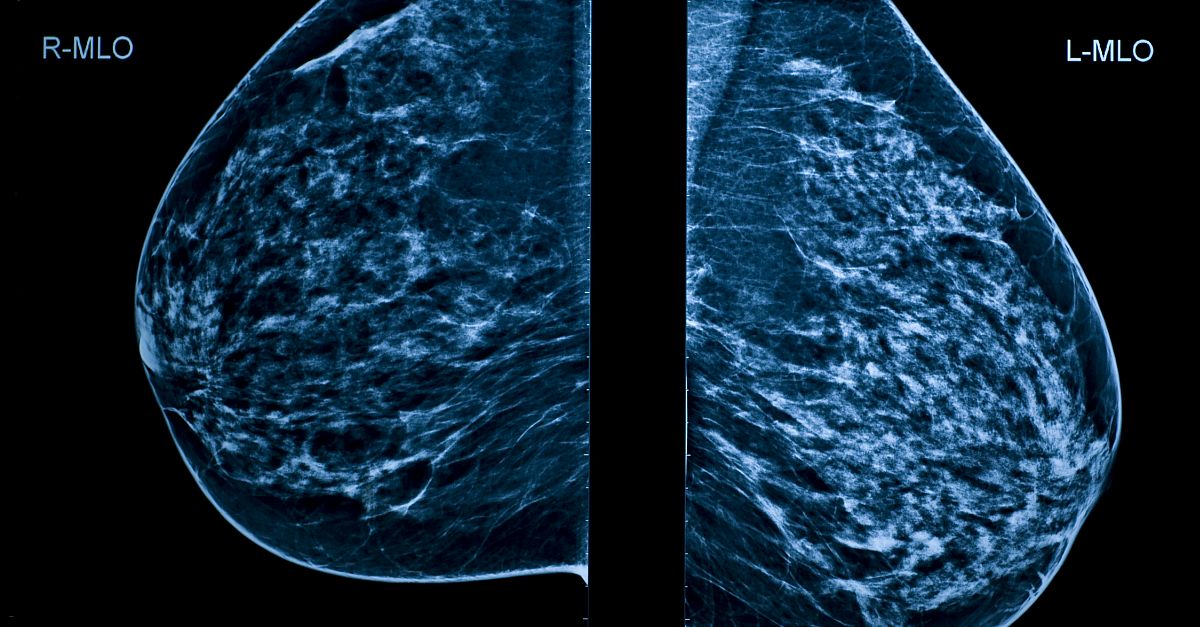
Widespread implementation of screening mammography has enabled earlier detection of breast cancer and subsequently improved outcomes. However, there are limitations to current processes, as global access to screening mammography is constrained by availability of specialized radiologists and the potential for variation in performance among human readers. To address these restrictions, artificial intelligence (AI) computer-aided detection (CAD) algorithms are gaining increased attention worldwide. An evaluation recently published in JAMA Oncology compared the results of 3 different AI CAD algorithms as readers of a large set of mammographic examinations. The retrospective case-control study included women aged 40 to 74 years from the Swedish Cohort of Screen-Aged Women data set, who were invited for screening examinations between 2008 and 2015. The final study sample included 8805 women, 739 of whom received a diagnosis of breast cancer. One AI CAD was found to reach—and in some comparisons surpass—the performance level of radiologists in assessing screening mammograms (81.9% sensitivity at 96.5% specificity). These results compare favorably with Breast Cancer Surveillance Consortium benchmarks (86.9% sensitivity at 88.9% specificity). Combining the first readers with the best AI CAD identified more positive cases than a combination of 2 human readers. When AI CAD assessments were used as the starting point, cancer detection increased by an estimated 8%, while abnormal assessments (true positives plus false positives) increased by 77%. Dr Mattie Salim et al suggest that a cost-benefit analysis of the addition of a first reader to the AI CAD algorithm would help to determine the economic implications of adding a human reader.
High level: Although AI CAD algorithms have not been approved for use as independent readers by the US Food and Drug Administration, these results suggest that a commercially available AI CAD algorithm should be further evaluated as an independent reader in prospective clinical trials to determine whether these results will translate to success in routine clinical practice. In a commentary, Dr Constance Dobbins Lehman notes that if AI models are proven able to reliably sort women with cancer detected on their mammograms from those without cancer, the life-saving potential of quality screening mammography could be made available and affordable to a large population of women globally who currently do not have access to adequate screening.
Ground level: Currently, every mammogram must be interpreted by a subspecialist, contributing to high costs and limiting access to screening for some women. It also introduces the potential for human error. The results of this study suggest that a commercially available AI CAD algorithm could perform at or above the level of radiologists and improve the effectiveness of breast cancer screening. However, AI CAD algorithms are unlikely to replace humans altogether. Rigorous, prospective clinical studies of AI CAD are needed to determine the optimal screening processes, but given the price of commercial AI systems, Dr Salim et al suggest that a realistic implementation may be 1 radiologist and 1 algorithm.