Dr Sushil Bhardwaj, from the Bon Secours Medical Group and Director of the Bobbi Lewis Cancer Program at Good Samaritan Hospital in Suffern, NY, USA, started his fellowship in neoplastic diseases at the Mount Sinai School of Medicine, New York, which at that time was chaired by James F. Holland, MD, the founder of Cancer and Leukemia Group B (CALGB). There he specialized in breast cancer and clinical trials under the aegis of CALGB. Since then, he has had a successful career in the community setting treating many types of cancer and serving as director of an American College of Surgeons-accredited cancer program, overseeing the implementation of and adherence to the standards of quality cancer treatment as set by the American College of Surgeons.
Dr Bhardwaj has authored several peer-reviewed publications and book chapters. He previously held academic appointments at Mount Sinai School of Medicine, New York Medical College, and Albert Einstein College of Medicine. Here is a recap of our conversation:
What recent advancements in the management of renal cell carcinoma do you consider the most relevant to clinical practice?
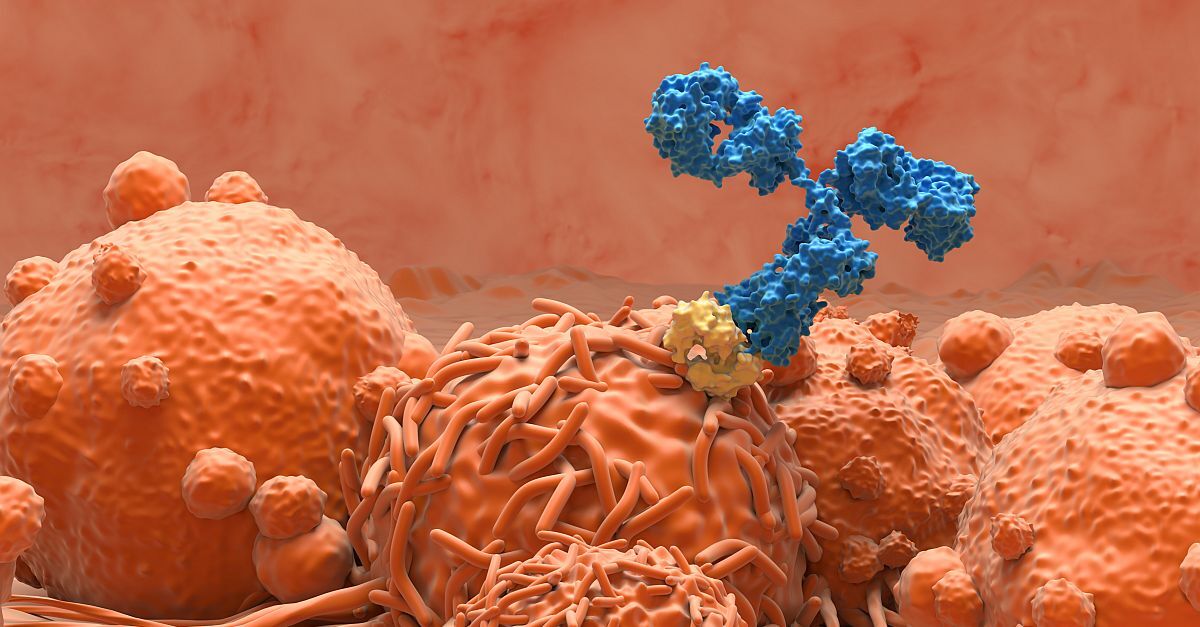
Precision medicine has been an important development, with greater understanding of the interplay between targeted therapies and the cancer and how the immune system fits in, and being able to exploit that interaction with immunotherapies. We now have better tools to support treatment decisions, such as the International Metastatic Renal Cell Carcinoma Database Consortium criteria for determining low risk, intermediate risk, or high risk, and we’ve made significant progress in improving survival. I have patients with renal cell carcinoma whom I have been treating for the last 10 to 15 years, and they are alive and doing reasonably well with currently available treatments. The big news earlier this year was a demonstrated improvement in overall survival with the use of an adjuvant immune checkpoint inhibitor such as pembrolizumab in patients with renal cell carcinoma. Most recently, the mature data for the combinations of different oral tyrosine kinase inhibitors (TKIs) with immune checkpoint inhibitors for advanced disease presented at the American Society of Clinical Oncology (ASCO) meeting in June showed a positive impact in terms of quality of life, tolerability, disease-free survival, and overall survival.
In your view, what represents the biggest challenge in managing renal cell carcinoma: diagnosis, treatment, patient education, or other factors?
In terms of diagnosis, more and more patients are being diagnosed when a mass is found on the kidney during imaging studies, particularly computed tomography scans, for reasons unrelated to a diagnosis of cancer. For those patients, a determination then needs to be made as to how significant it is and whether it is renal cell carcinoma or benign. Sometimes that is feasible based on the radiographic characteristics, but very often it is not, and there are issues in trying to establish a diagnosis with a biopsy, since renal cell carcinomas can be very vascular.
The main challenge in terms of treatment is cost/financial toxicity. Several of these therapies are not cheap, and lack of health insurance affects our ability to treat all our patients across a diverse population. Many patients don’t make it to clinical trials or to academic centers due to lack of insurance. To me, that remains a challenge as it relates to treatment, because those patients may not be represented in clinical trials. The US Food and Drug Administration is increasing its focus on making our clinical trials more inclusive and diverse, and ASCO has recognized that over the last several years as well.
As far as patient education, it’s very important to be able to use the physician extenders (eg, physician assistants, nurse practitioners) to provide patient education, particularly regarding side effects and their management, since some of these drugs have complex side effects.
Which emerging trends or approaches do you believe hold the most promise for advancing the treatment of renal cell carcinoma?
One development, that I find promising is a noninvasive way to differentiate renal cell carcinoma from a lesion that might be benign. There is a new positron emission tomography imaging technique that is being investigated in a phase III trial using an antibody against carbonic anhydrase IX, which is expressed in renal cell carcinoma. I think if that pans out and gets approved, it would be an important new development for diagnosis and for treatment planning. Another potential advancement is the use of kidney injury molecule-1 (KIM-1) to help identify patients who may have better response to the use of an immune checkpoint inhibitor in the adjuvant setting. We may also be able to use it to measure molecular residual disease and for monitoring our patients with renal cell carcinoma. That has potential to be very helpful in terms of being able to determine which patients might benefit from the use of an immune checkpoint inhibitor in the adjuvant setting.
What remains an unmet need in renal cell carcinoma?
One unmet need is building off data from an article published in the New England Journal of Medicine that reported overall survival with the use of pembrolizumab in the adjuvant setting. When those patients experience disease progression or if the cancer comes back—which happens in about one-third of patients—what do we do next? There is a data gap in the care of these patients, and there are very little data about sequential use of immune checkpoint inhibitors. If someone has had an immune checkpoint inhibitor in the adjuvant setting and then has progression, we don’t yet know when we can use it again, or if it will be effective if we do use it again. We also need better understanding of where the oral TKIs fit in as we start to use adjuvant immune checkpoint inhibitors.
How do you see the field evolving in the next 3 to 5 years?
I think we will have better treatments and a better understanding of when to apply those treatments, perhaps based on KIM-1 or maybe another biomarker to avoid overtreatment.
As I said before, these therapies are expensive, and they all have different side effects, so I believe we will need to find better ways to apply them in a more targeted fashion.
What is the value of a membership to the Axess Network for community oncologists?
I joined the Axess Network in September 2013, and I’ve been very fortunate to participate in meetings that were organized by the Axess Network and subsequently, to become a moderator for some of those meetings since. I always walk away from those meetings having learned something new, but more importantly, what I hear from my colleagues out in the community is that these meetings are great opportunities for an individual medical oncologist/hematologist to level set their practice and compare it with that of their colleagues in different parts of the same community, in different parts of the state, in different parts of the country, and in other countries. It can help validate their own practices and help them learn new information in a manner that is very conducive to a free exchange of ideas. The interaction between KOLs and participants has been exciting for me to watch as a moderator, because the faculty members also learn a lot from the community physicians in a relatively intimate setting of a small group of people. The participants acquire knowledge that helps them take better care of their patients, and that’s really what it’s all about . . . to get that information out to the community physicians so they can take better care of their patients.