Immune checkpoint inhibitors have demonstrated efficacy in multiple solid and hematologic malignancies over the past 10 years, and continue to redefine the course of therapy for many patients. They work by helping the immune system recognize and kill foreign targets and overcome the immunosuppressive tumor microenvironment. However, their use may be limited by adverse events of varying degrees of severity. Additionally, when used as monotherapy, disease control with immunotherapy is short-term, and there are many patients for whom checkpoint inhibitors are ineffective. Therefore, current research is aimed at determining biomarkers that will predict response, exploring alternative treatment strategies (ie, rechallenge), and identifying rational combinations that can improve objective response rates or prolong disease control. In a recent Lancet review article, Dr Funda Meric-Bernstam and colleagues summarized this research and discussed the rationale for the combination of immune checkpoint inhibitors with different treatment strategies.
Generally, understanding of biomarkers of sensitivity and resistance to immunotherapy is low. The most studied predictive marker for immune checkpoint inhibitors is programmed cell death protein 1 ligand 1 (PD-L1), which is now routinely used to determine whether to give immunotherapy in several tumor types. Other biomarkers being explored are tumor mutation burden (TMB), neoantigens, CD8 positivity, certain genes, and tumor characteristics such as gene mutations and pathway activation. In addition, early tumor response monitoring has gained increasing attention; one potential predictor of response is an early drop in mutant allelic frequency in cell-free DNA.
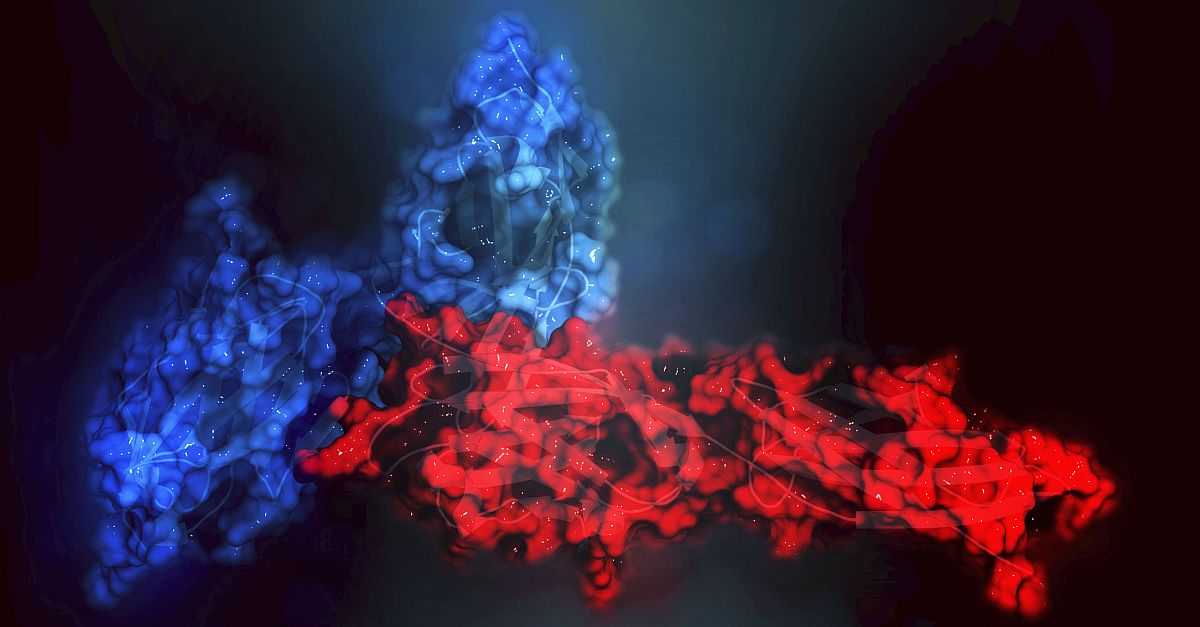
Tumors that are responsive to immune checkpoint inhibitors are often referred to as “hot tumors”; therefore, a key strategy behind combination therapy is to turn so-called “cold tumors” to hot. There are numerous combination strategies being pursued in clinical trials that combine immune checkpoint inhibitors with multiple types of treatments, such as chemotherapy, radiation therapy, vaccines, intratumoral strategies, targeted therapies, and others. Unfortunately, while it is believed that these combinations may enhance efficacy, they can also increase toxicity, and most of the combinations that have been tested were unsuccessful. To address the toxicity concern, some researchers are analyzing sequential combinations of immunotherapy. For example, a team at Moffitt Cancer Center is investigating sequential combinations of immunotherapy followed by either BRAF/MEK-targeted therapy or another combination in patients with advanced melanoma. Their research showed that immunotherapy followed by targeted therapy was more effective than either approach alone. With all of the ongoing research, new insights and discoveries are expected to continue to reshape the treatment of immunoresponsive tumor types over the next decade and beyond.
High level
There are regulatory and cost challenges that will impact the future of immunotherapy combinations. Some combinations may unnecessarily increase the overall cost of care without improving outcomes in patients who would have had prolonged responses with monotherapy. Dr Meric-Bernstam and colleagues recommended a programmatic approach to developing a framework for biomarker-driven combination immunotherapy. Researchers should consider designing some trials that investigate use of immune checkpoint inhibitors and combinations earlier in the treatment pathway, as opposed to waiting until failure of monotherapy. In particular, some combinations may have greater efficacy in patients who are immunotherapy naive vs those who are immunotherapy resistant. Immunotherapy may be less effective in later lines of therapy, and some patients may have mechanisms of resistance that might be irreversible, so detailed studies are needed to identify not only which patients would benefit from combination therapy, but also when to initiate specific combinations for optimal results.
Ground level
Toxicity is an important consideration when looking at novel combinations, as not all drugs can be safely combined with immune checkpoint inhibitors. The researchers at Moffitt Cancer Center have found that sequential treatment approaches may be clinically beneficial. In determining when to use these combinations, oncologists will need to consider which to use, as well as how to select optimal combination partners. Patient workups in the future may include an integrated analysis of tumor genomics, immune profiling, and peripheral blood analysis to understand the immune state of the tumor and personalize therapeutic choices.