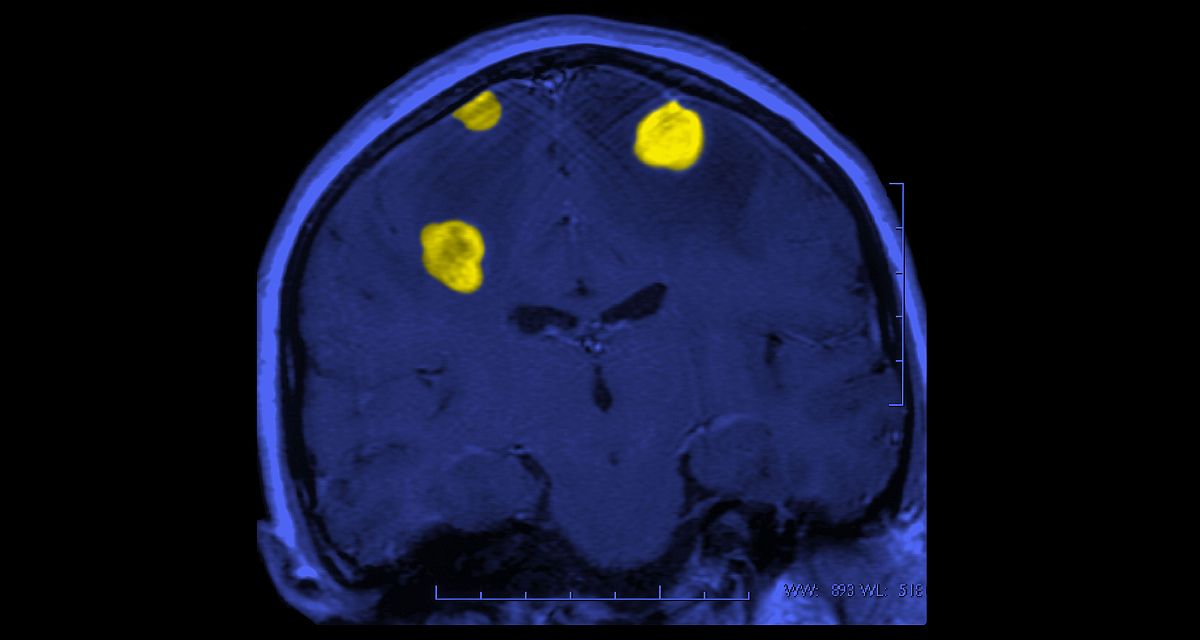
Once considered an end-stage progression of cancer to be managed palliatively, brain metastasis is increasingly being treated with more-aggressive approaches. As treatments are advancing and outcomes improving, 3 physicians from Memorial Sloan Kettering Cancer Center (MSKCC) in New York City propose that brain metastasis should be treated as a distinct oncologic disease managed by an integrated multidisciplinary team, as reported in a recent JAMA Oncology Viewpoint article.
New central nervous system (CNS)-active drug approvals—including tyrosine kinase inhibitors targeting the EGFR gene variant, ERBB2 (formerly HER2 or HER/neu)-amplified and ALK-rearranged cancers, plus checkpoint inhibition activity in CNS melanoma—are a key driver of improved outcomes for many patients with brain metastasis. Wider application of stereotactic radiosurgery has also improved outcomes and reduced radiation-induced cognitive adverse effects commonly seen after whole-brain radiation regimens.
While these advances in treatment create a welcome challenge, they have made decision-making in the management of brain metastasis ever more complex. As a result, specialized attention and integrated multidisciplinary programs are critical to offering the necessary perspectives and expertise to individual patient cases. The authors advocate for multidisciplinary teams organized around CNS involvement to provide coordinated decision-making and to help close potential treatment gaps leading to worse oncologic outcomes. Interrelated elements of effective brain metastasis programs include dedicated tumor boards, multidisciplinary outpatient clinics, inpatient service lines, and clinical trial work groups.
High level
Recognizing the unique challenges and opportunities of managing brain metastasis is essential for continued improvements in the care of these patients. Inpatient multidisciplinary teams that provide consultation services and rapid, coordinated decision support can spark workflow improvement for the management of brain metastasis across the inpatient-outpatient continuum. Additionally, giving community healthcare professionals access to CNS tumor board meetings can arm them with expert decision support by medical oncologists, neuro-oncologists, or CNS-focused radiation oncologists, therefore expediting appropriate treatment.
Ground level
Patient outcomes can be improved, and ecosystems created, by accessing individuals who possess the unique level of expertise and coordination necessary for treating brain metastasis as a distinct disease. For this to happen, full participation of medical oncologists on brain metastasis tumor boards is essential, albeit not always possible. The authors recommend utilizing a virtual platform to preschedule specific patient discussions and facilitate the engagement and coordination of optimal patient care.